Key Takeaways
-
Telehealth’s rapid growth and market potential in 2025
-
The role of video streaming in delivering real-time, high-quality care
-
Innovations like AI and RPM are transforming virtual healthcare
-
The financial and operational benefits of video-powered telehealth
-
Technology, infrastructure, and security are shaping the telehealth experience
-
Policy changes and future trends driving adoption
Telehealth's Explosive Growth: Context & Impact
Enough evidence is available to realize the growth potential of telehealth, indicating a global shift towards virtual healthcare. By the end of 2026, it is projected that 25–30% of all medical visits in the U.S will take place through telemedicine. This transformation is driven by the growing demand for convenient and accessible healthcare options and advancements in technology that facilitate virtual consultations.
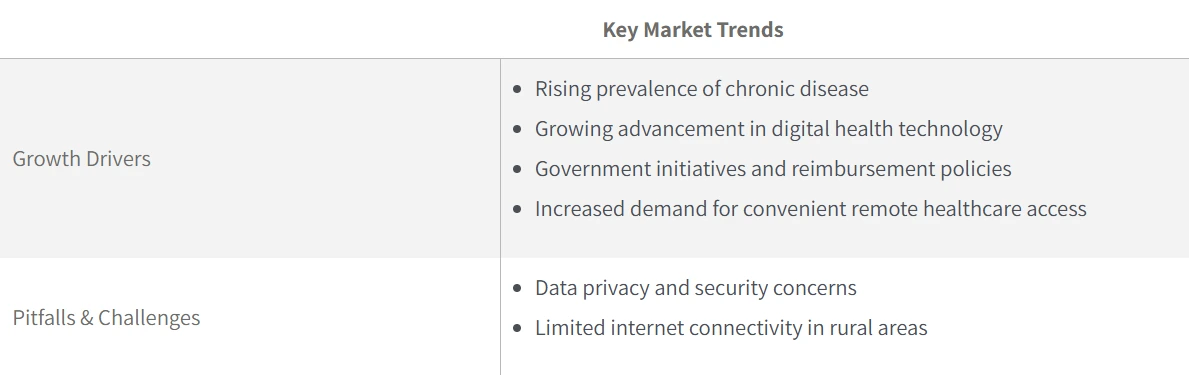
Crucially, this surge has been accelerated by supportive government action. During the pandemic, regulatory waivers eliminated key barriers, enabling healthcare providers to offer virtual care more widely and making it easier for patients to access services from home. The positive outcomes reported by both patients and caregivers highlighted the effectiveness of these initiatives.
In the U.S., the American Hospital Association (AHA) has since pushed to extend and expand such reforms, lifting geographic restrictions, increasing the telehealth workforce, and ensuring fair reimbursement rates. These policy efforts have not only maintained the momentum sparked during the pandemic but also emphasized the importance of equitable access to health care, directly fueling telehealth’s long-term market growth.
This upward trajectory reflects a combination of expanding patient demand, chronic disease management needs, greater comfort with virtual care, and a policy environment increasingly designed to sustain and scale telehealth.
Virtual Visit: A New Standard in Medical Care
Virtual visits are allowing patients to consult with physicians about their medical history and discuss new prescriptions from the comfort of their homes. This shift has made health care more accessible and convenient, particularly for those living in remote areas or with mobility issues, addressing many frequently asked concerns related to remote care, sinus infections, preventive care, and physical exams.
The integration of video streaming technology in telehealth has significantly increased the frequency of doctor-patient consultations. Millions of patients are expected to use these services in the coming years, reaping the benefits of timely medical advice and treatment. A live visit has proven more efficient, reducing the average time spent compared to traditional in-person appointments.
Enhancing Mental Health Support
Video consultations are improving mental health by offering a convenient platform for therapy, with visual cues aiding diagnosis. While some patients feel less personal connection or notice provider distractions, many appreciate the comfort and reduced anxiety of virtual sessions. This convenience boosts digital patient engagement and retention. Clear communication remains essential to ensure patients feel heard and understood during telehealth visits.The Healthcare Advantage: Why Video Streaming Is Essential?
Telehealth leverages digital technologies to access healthcare services remotely. It includes practices ranging from transferring medical information for clinical and educational purposes to enabling direct interactions between patients and health care providers. Central to this revolution is video streaming, which enhances remote patient diagnostics and treatment by creating real-time, face-to-face interactions online using telehealth tools.
-
Real-Time Care, Anywhere: High-quality video allows clinicians to observe visual cues, rash, respiration, and gait that are critical for diagnosis. With 5G and cloud-based platforms, lag is nearly eliminated, making video consults feel almost in-person.
-
Enhanced Reach & Rural Access: Real-time communication solutions have significantly improved access to telehealth, enabling individuals to receive medical advice and treatment without travelling long distances. In underserved or rural areas, video consultations are now a lifeline, boosting equity.
-
Patient & Provider Satisfaction: Telehealth sees growing buy-in, with around 59% of providers saying it improves access. Patient satisfaction rates average 82%, and about 65% of providers now offer hybrid models, blending virtual and in-person care, says Market Growth Reports.
-
Scheduling telehealth appointments is remarkably convenient: Patients can simply download an app or visit a website to book a virtual doctor appointment. Often covered by insurance and offered at reduced costs, these virtual visits make health care more affordable and accessible. During an online health consultation, primary care providers can also bring in specialists in real time, ensuring patients receive comprehensive, coordinated medical advice without multiple appointments.
Video-Driven Innovation: RPM, AI, and Beyond
Telehealth in 2025 isn’t about seeing your doctor through a screen; it’s about making every interaction smarter. Video platforms are becoming healthcare hubs, combining remote monitoring tools, AI-driven insights, and advanced diagnostics to improve care and speed.
Integration With Wearables & Remote Patient Monitoring
Wearables are becoming an extension of video consults. Integration with Wearables & RPM grew 70% between 2019 and 2022. RPM, supported by video streaming and other technologies, enables continuous observation of vital signs, allowing primary care providers to offer timely interventions for conditions like high blood pressure. Providers can adjust treatment plans as needed by closely monitoring these metrics, ensuring optimal patient outcomes. Wearable devices are instrumental in this process, recording physiological data in real-time. These devices:-
Collect crucial health information such as heart rate, blood pressure, and activity levels.
- Transmit this data to the healthcare provider for analysis.
- Provide a continuous data flow that helps in the early detection of potential health issues.
- Allow for prompt medical attention based on the data collected.
Primary care visits complement remote monitoring by providing a platform for ongoing clinical assessment and consultations. Patients can discuss their health metrics with their primary care providers, who can make necessary adjustments to their treatment plans. This combination of real-time data and direct communication ensures a comprehensive approach to patient care.
The integration of RPM and video streaming not only enhances the patient experience but also supports a more proactive approach to healthcare. By leveraging these technologies, primary care providers can deliver more personalized and effective care, ultimately improving patient outcomes and satisfaction.Artificial Intelligence in Telehealth Platforms
Artificial intelligence (AI) is transforming telehealth by enhancing the accuracy and efficiency of medical diagnoses. AI algorithms analyze images and patient data, supporting doctors in their interpretations and improving overall diagnostic accuracy. AI tools embedded in video platforms now assist with diagnostics, documentation, and triage. One cutting-edge development, CardioLive, can extract heart rate from streaming video and audio with striking precision (1.79 BPM mean error), outperforming older methods by over 69% and 81%. AI also contributes to personalized interactions during telehealth consultations. By analyzing individual patient records, AI systems can provide timely and personalized communications, enhancing patient engagement and satisfaction. This level of personalization ensures that patients receive care tailored to their specific needs. Moreover, AI technologies linked to monitoring devices allow for real-time tracking of health metrics. These systems can alert health care providers to any anomalies, enabling timely interventions and adjustments to treatment plans. This real-time monitoring is crucial for managing chronic conditions and improving patient outcomes. AI’s ability to manage numerous patient interactions simultaneously helps scale telehealth services, making healthcare more accessible. By overcoming geographical barriers and matching care providers’ availability with clinical needs, AI ensures that more patients can receive quality care regardless of their location.The ROI of Care: The Financial Case for Video Telehealth
Telehealth isn’t just revolutionizing access to care – it’s transforming the economics of healthcare delivery. The cost savings and efficiency gains are compelling for both providers and patients. The following industry statistics indicate why video telehealth makes financial sense:
-
Telehealth can lead to cost savings of up to $130 billion annually in the US healthcare system.
-
Reduction in hospital readmissions by 20% and emergency visits by up to 30%.
-
Telehealth visits cost 20% less than in-person care, saving patients roughly 30 minutes per appointment.
-
Moreover, telehealth consultations for postoperative follow-up have resulted in a 30% reduction in hospital visits, decreasing patient burden and healthcare costs. Telehealth services expansion contributed to a 15% reduction in no-show rates among outpatient clinics during 2021.
Infrastructure & Security: The Foundations of Video Telehealth Technology
Reliable Networks as the Backbone
Just as streaming services have invested in stronger infrastructure to deliver smoother, higher-quality video, telehealth also relies on robust networks. The lesson from media platforms is clear: improved bitrate, reduced lag, and reliable connections aren’t just about convenience; they’re essential for patient trust and clinical accuracy.Security and Electronic Health Record Integration
Beyond connectivity, security and compliance are non-negotiable. Addressing privacy concerns is crucial for the widespread adoption of telehealth services, ensuring that patients feel confident in the security of their data. Both primary care providers and patients must use secure connections and devices to maintain the integrity of video consultations. Modern telehealth platforms must meet HIPAA, GDPR, and other data protection standards. Encryption and seamless integration with electronic health records (EHRs) ensure that video consultations become a natural extension of a clinician’s workflow, secure, efficient, and fully aligned with health care protocols.What's Ahead: The Telehealth Ecosystem of Tomorrow
The evolution of telehealth is no longer a short-term response to a crisis; it’s becoming a permanent fixture of healthcare delivery. The ecosystem ahead will be shaped by regulatory reforms, advanced technologies, and patient expectations for seamless, secure, and equitable access to care.
Regulatory Momentum & Expanded Access
Policy is moving telehealth forward. In the U.S., the Telehealth Modernization Act of 2024 (H.R. 7623) extends Medicare flexibilities (e.g., audio-only visits, no in-person requirement) through 2025, impacting 62 million beneficiaries. These changes support rural clinics and chronic care access via video.
Key flexibilities now extended through 2025 include Medicare home visits, audio-only options, and expanded provider eligibility for rural and underserved areas. Behavioral health access is becoming permanent, with no geographic limits and broader provider coverage, cementing telehealth as a core part of U.S. healthcare.
Technology Drivers of Change
On the other hand, technology is rapidly evolving to redefine the patient experience:
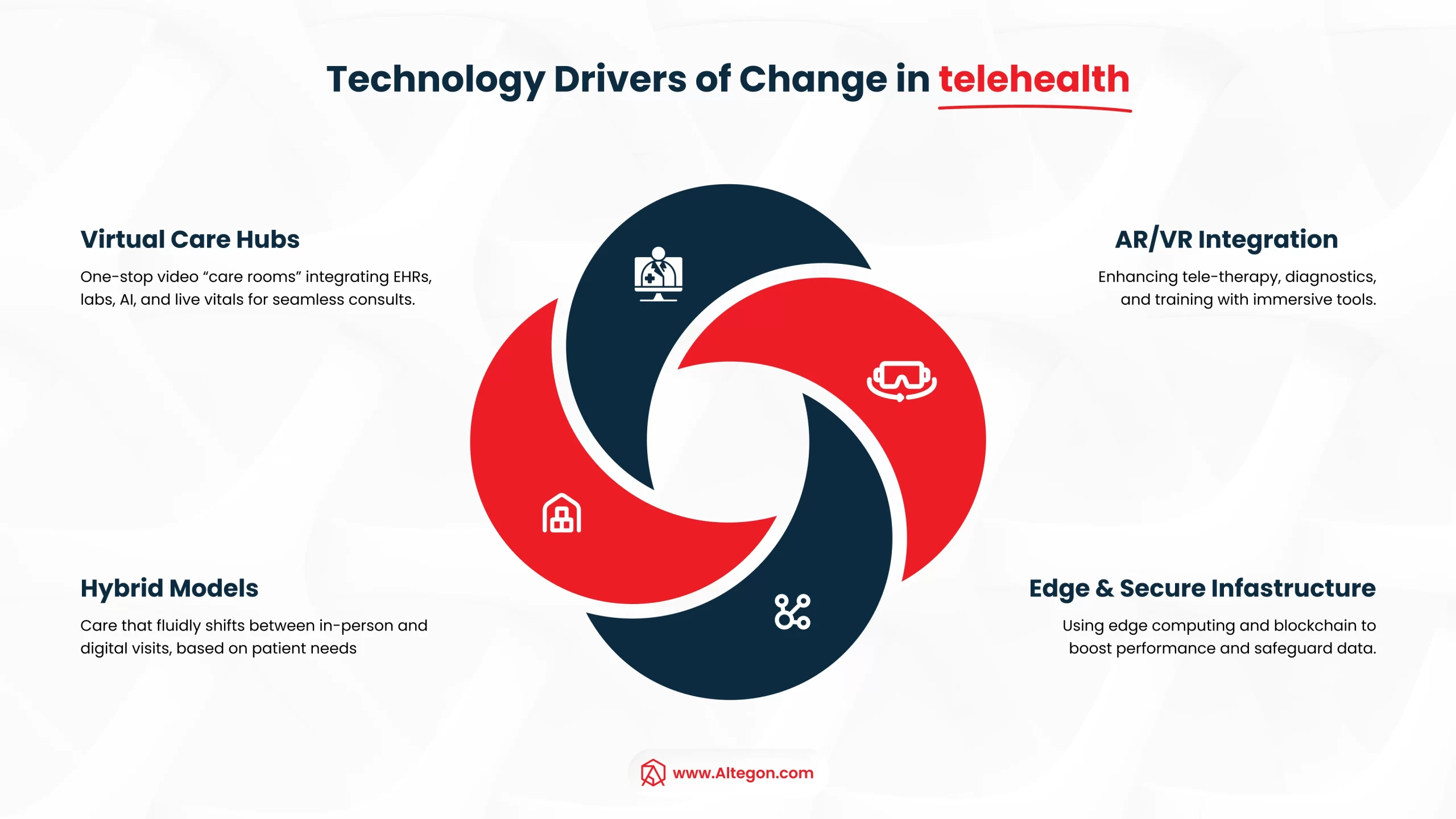
- Virtual Care Hubs: One-stop video “care rooms” integrating EHRs, labs, AI, and live vitals for seamless consults.
- Hybrid Models: Care that fluidly shifts between in-person and digital visits, based on patient needs.
- AR/VR Integration: Enhancing teletherapy, diagnostics, and training with immersive tools.
- Edge & Secure Infrastructure: Using edge computing and blockchain to boost performance and safeguard data.
Together, policy and technology are shaping a telehealth ecosystem built for scale, security, and patient-centered care.





Comments are closed.